3 mSv:
Annual natural background radiation dose in US
Women as One would like to recognize the contributions from Sheila Sahni MD, FACC, FSCAI,
Alaide Chieffo, MD, FESC and Stephen Balter PhD, FAAPM, FACMP, FACR, FSCAI, FSIR for their work on “Radiation Safety in the Practice of Cardiology”
Sheila Sahni, MD, FACC, FSCAI
Alaide Chieffo, MD, FESC
Stephen Balter, PhD, FAAPM, FACMP, FACR, FSCAI, FSIR
Women as One would like to recognize our global partners for their endorsements.
Together, we can amplify our voices to create meaningful change to support women around the world.
WHAT THE PREGNANT CARDIOLOGIST NEEDS TO KNOW
(CONSIDERATIONS/GAPS)
RADIATION BASICS AND PROTECTION
RECOMMENDATIONS

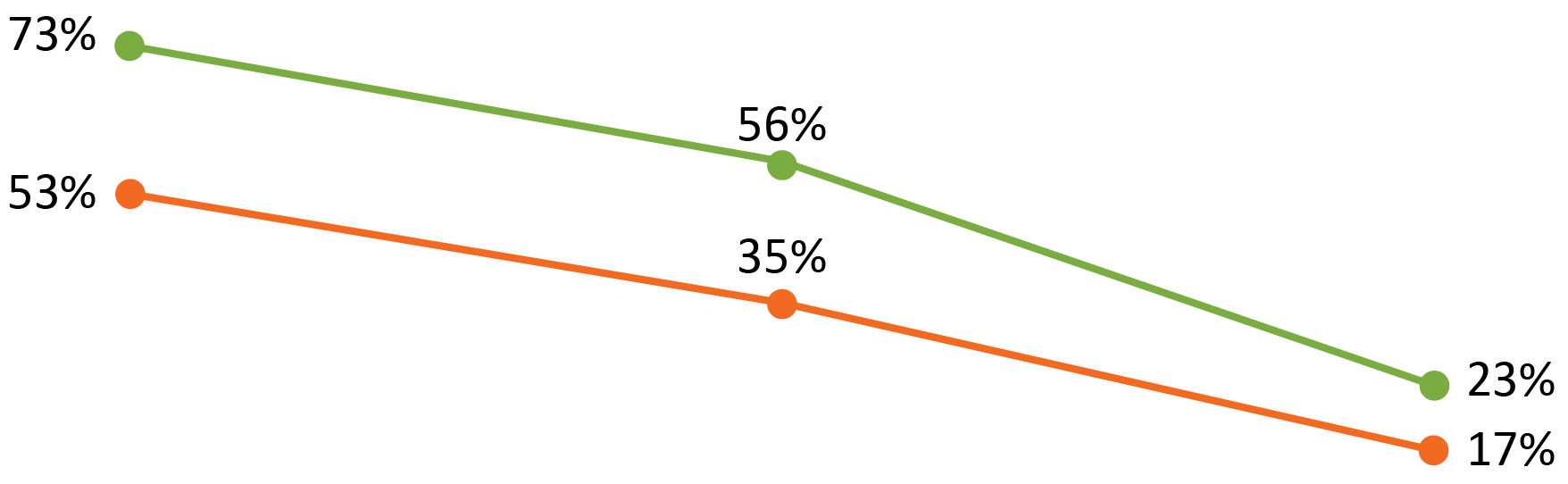
Lewis, S.J. et al. J Am Coll Cardiol. 2017;69(4):452-62.
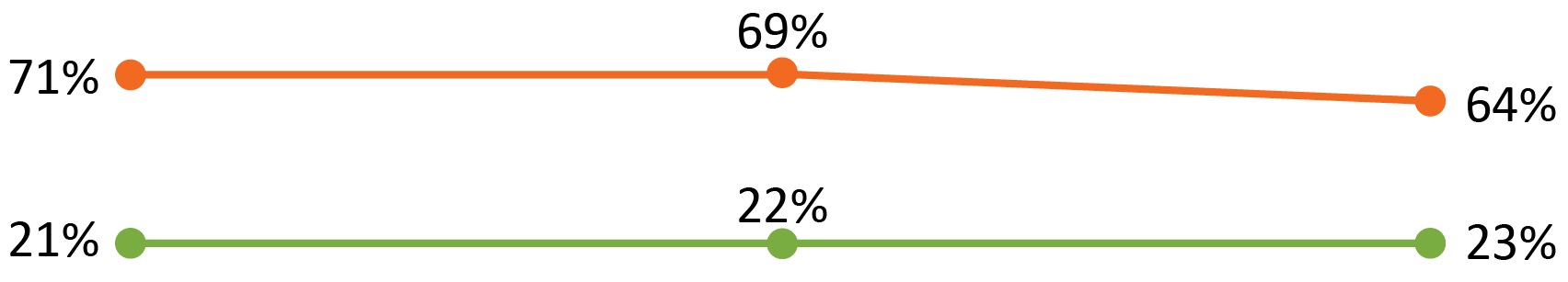
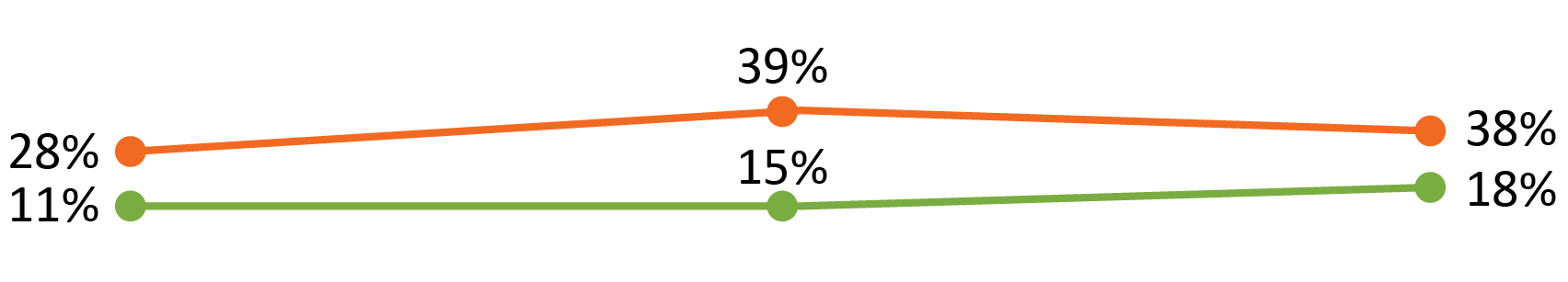
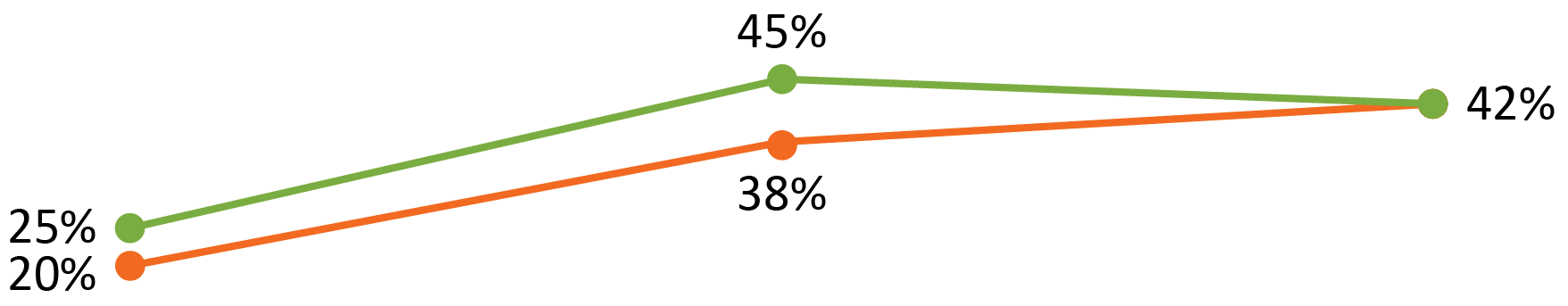
Areas for which there has been minimal or no change in responses to survey questions regarding personal and professional life issues are contrasted with areas where significant changes have occurred.
Sarma A, et al JACC 2017;69:92
Women are often asked whether they intend to have children during interviews
A career in cardiology often impacts family planning
Female cardiologists avoid pregnancy during periods of radiation exposure
Women underutilize radiation reduction and monitoring strategies
Cardiologist experience a high incidence of pregnancy complications
Pressure to take shorter parental leave
Women do not meet their breastfeeding goals
Avoid such questions
Offer all candidates information on parental leave policies
Recognize the importance of pregnancy, parental leave, and breastfeeding
Include radiation exposure recommendations in fluoroscopy training
Connect cardiologists with radiation safety officer
Provide maternity lead and fetal dosimeters
Parental leave of 2 months for all cardiologists (men and women) with flexibility to account for potential complications
Optimize space, me, and culture acceptance for women to express milk in the workplace
Sarma, A.A. et al. J Am Coll Cardiol. 2017;69(1):92-101.
Y. Morishima, K. Chida, Y. Katahira, et al. Need for radiation safety education for interventional cardiology staff. Acta Cardiol, 71 (2016): 151-155
G. Sadigh, et al. Radiation safety knowledge and perceptions among residents. Acad Radiol, 21 (2014): 869-878
Catheterization and Cardiovascular Interventions 77:232–241 (2011)
Dauer, L.T et al. J Vasc Interv Radiol 2015; 26:171–181
Dauer, L.T et al. J Vasc Interv Radiol 2015; 26:171–181
Manzo et al. EuroIntervention 2022;18-online publish-ahead-of-print November 2022
Dauer, L.T et al. J Vasc Interv Radiol 2015; 26:171-181
Sarcozy A. Occupational radiation exposure in the electrophysiology laboratory with a focus on personnel with reproductive potential and during pregnancy: A European Heart Rhythm Association (EHRA) consensus document endorsed by the Heart Rhythm Society (HRS) Europace (2017) 19, 1909-1922. doi:10.1093/europace/eux252
Dauer, L.T et al. J Vasc Interv Radiol 2015; 26:171–181
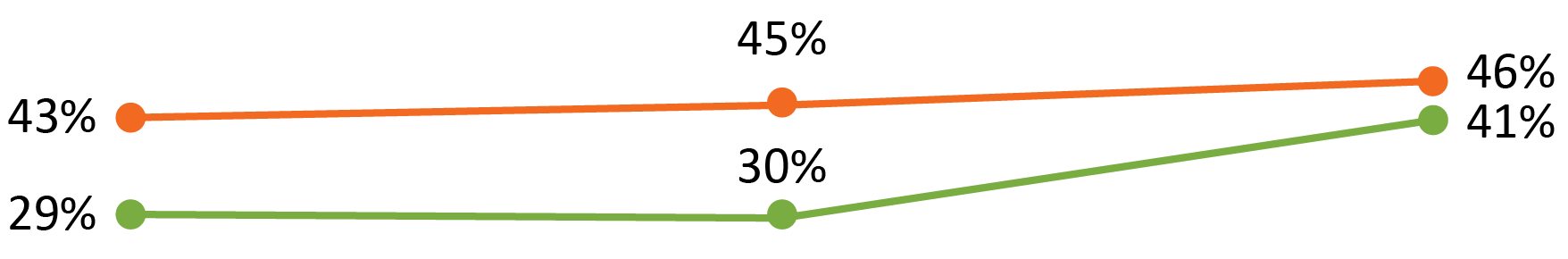
RECALL: US NRC Regulatory equivalent dose limit is 5mSv during the entire pregnancy of the declared pregnant woman
There is no evidence that radiation dose to the fetus < 100mGy during pregnancy is associated with an increased incidence of congenital malformation, stillbirth, miscarriage, growth malformation or mental disability
No statistically significant or convincing evidence of an increased risk of cancer in offspring of female radiation workers
Dauer, L.T et al. J Vasc Interv Radiol 2015; 26:171–181
Bhatt, D. et al. Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease; 2015
European Council. Council Directive 2013/59/Euratom of 5 December 2013 laying down basic safety standards for protection against the dangers
arising from exposure to ionizing radiation, and repealing Directives 89/618/Euratom, 90/641/Euratom, 96/29/Euratom, 97/43/Euratom and
2003/122/Euratom. Official Journal of the European Union 2014;57:1–73.
Overview of the current EU regulations and their local application demonstrating a general trend in more restrictive applicative directives usually limiting access to the catheterisation/electrophysiology lab and allowing a discretional power to the X-ray surveillance experts.
Manzo S et al. EuroIntervention 2022;18-online publish-ahead-of-print November 2022
Manzo S et al. EuroIntervention 2022;18-online publish-ahead-of-print November 2022
Manzo S et al. EuroIntervention 2022;18-online publish-ahead-of-print November 2022
Main deterministic/stochastic irradiation effects on the embryo/fetus at each pregnancy stage.
Sarcozy A et al. Europace (2017) 19, 1909–1922. doi:10.1093/europace/eux252
Manzo S et al. EuroIntervention 2022;18-online publish-ahead-of-print November 2022
Kneale GW et al. J Natl Cancer Inst. 1976;57:1009-14. 30.
Wagner LK et al. Medical Physics. 1998;25: 1557-8. 31.
Jablon S et al. Lancet. 1970;2:1000-3. 32.
Wagner LK et al. Radiology. 1982; 145:559-62.
Sarcozy A et al. Europace (2017) 19, 1909–1922. doi:10.1093/europace/eux252
Manzo S et al. EuroIntervention 2022;18-online publish-ahead-of-print November 2022
Dauer, L.T et al. J Vasc Interv Radiol 2015; 26:171–181
Kneale GW et al. J Natl Cancer Inst. 1976;57:1009-14. 30.
Wagner LK et al. Medical Physics. 1998;25: 1557-8. 31.
Jablon S et al. Lancet. 1970;2:1000-3. 32.
Wagner LK et al. Radiology. 1982; 145:559-62.
Sarcozy A et al. Europace (2017) 19, 1909–1922. doi:10.1093/europace/eux252
Manzo S et al. EuroIntervention 2022;18-online publish-ahead-of-print November 2022
Manzo et al. EuroIntervention 2022;18-online publish-ahead-of-print November 2022
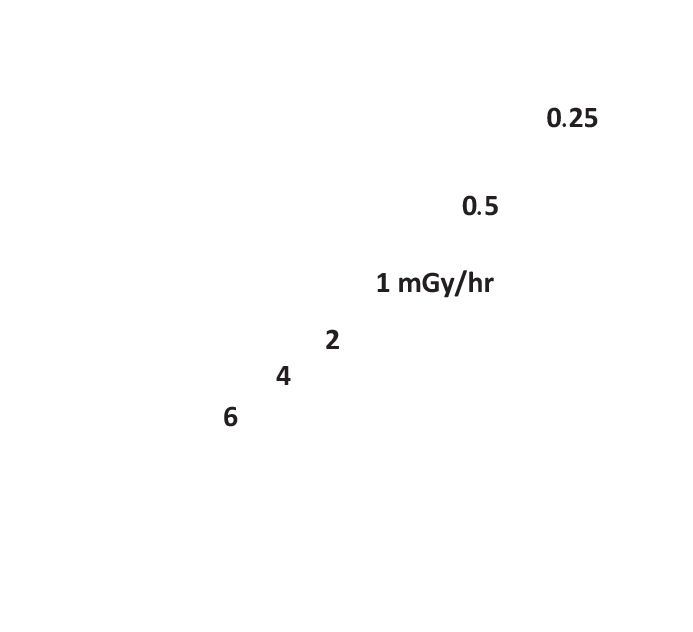
Annual natural background radiation dose in US
Legal dose limit for entire gestation
Under-lead dose to working pregnant interventionalist over entire gestation
How much fetus of working pregnant interventionalist estimated to receive over entire gestation
Known threshold for fetal injury
* Please note, legal and natural dose limits are based on US data. Limits vary by country
Ghatan C and Kothary N. Radiation Safety Considerations for the Female Interventionist. Endovascular Today. August 2016
Brent RL. Clin Perinatol 1986;13:615-48
Catheterization and Cardiovascular Interventions 77:232–241 (2011)
Manzo S et al. EuroIntervention 2022;18-online publish-ahead-of-print November 2022
Brent RL. Clin Perinatol 1986;13:615-48
Catheterization and Cardiovascular Interventions 77:232–241 (2011)
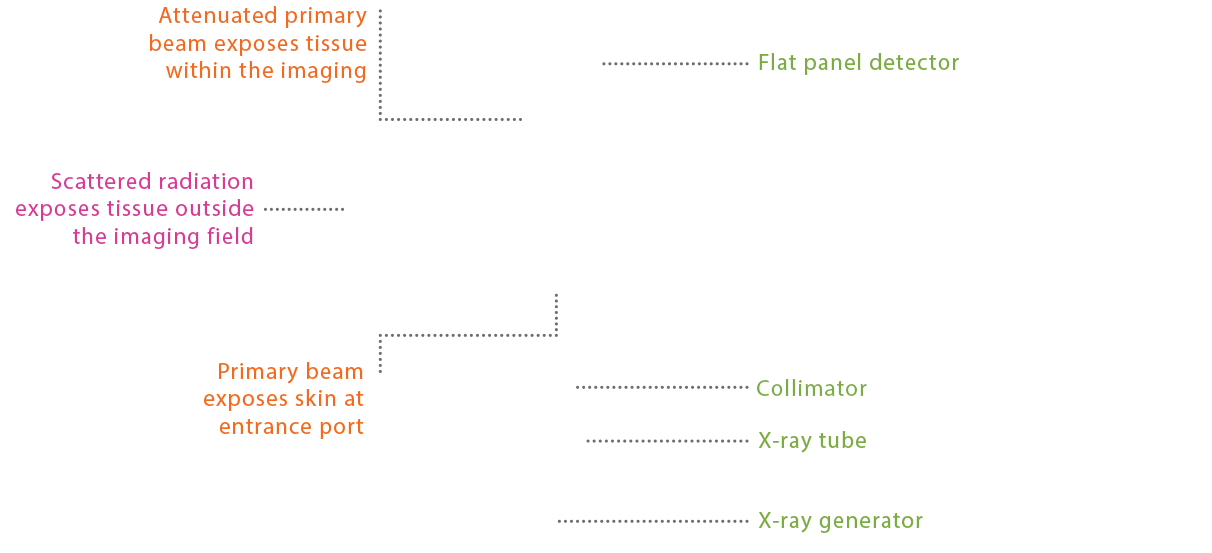
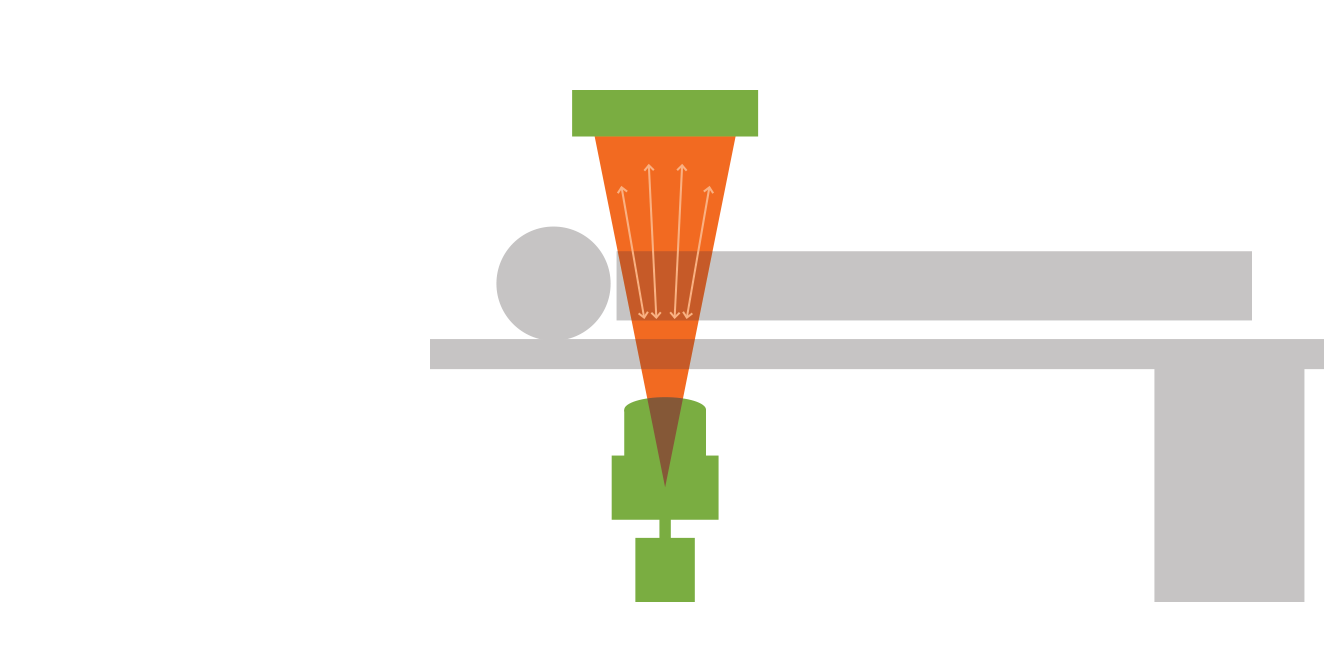
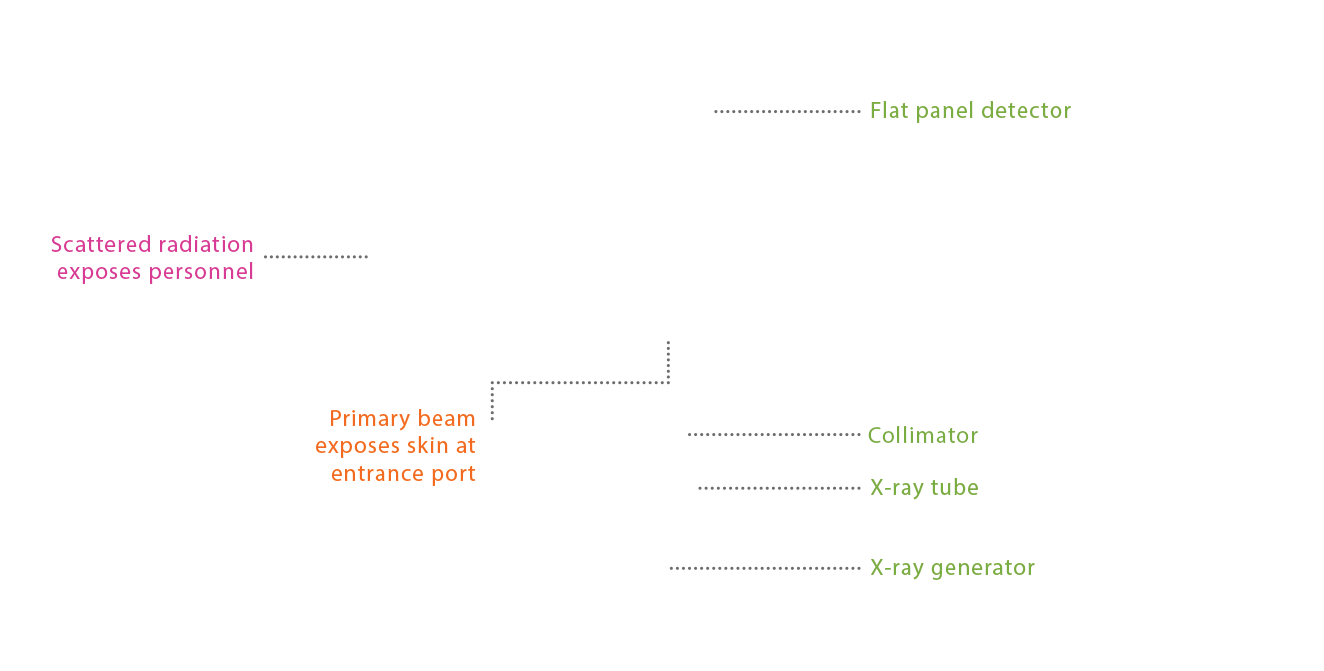
SPEND LESS TIME ON THE PEDAL
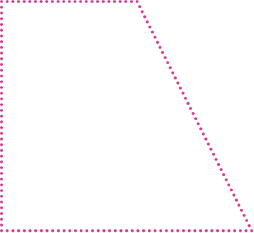
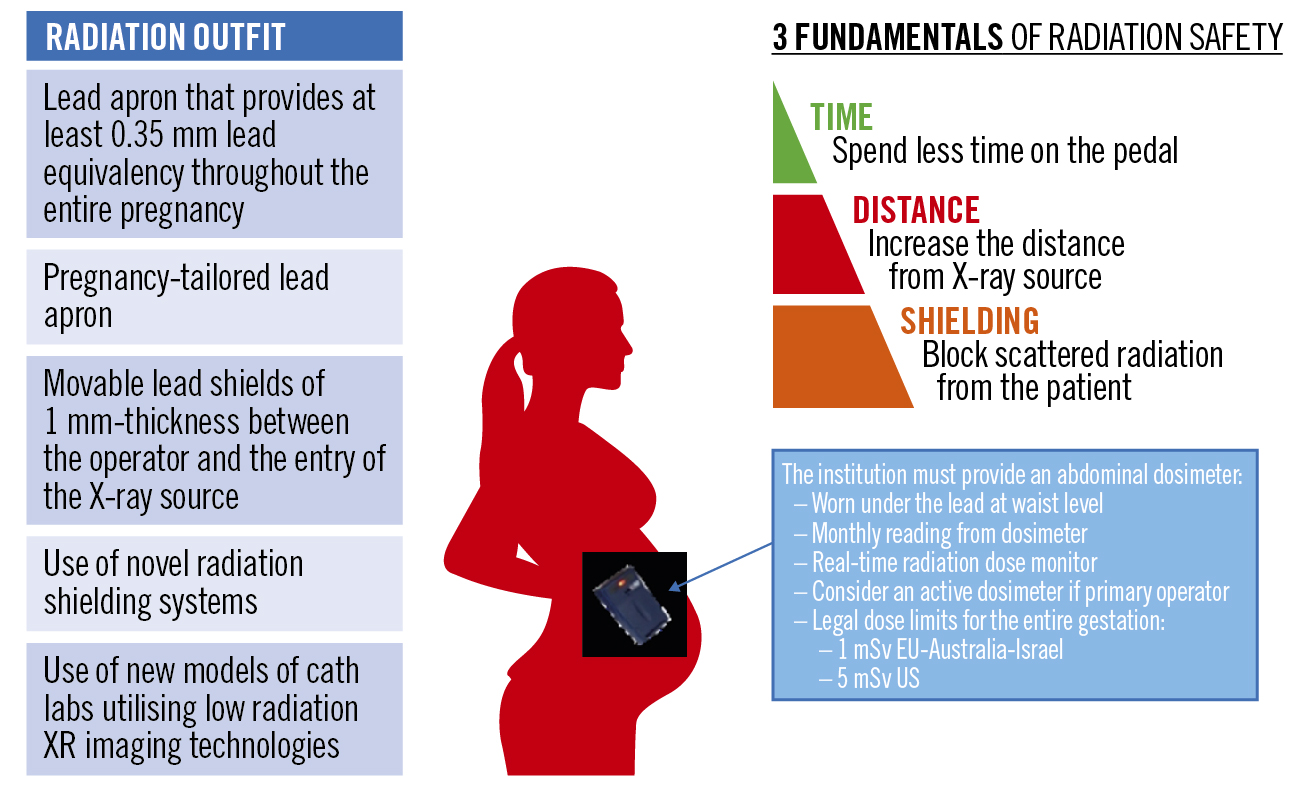
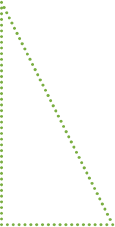
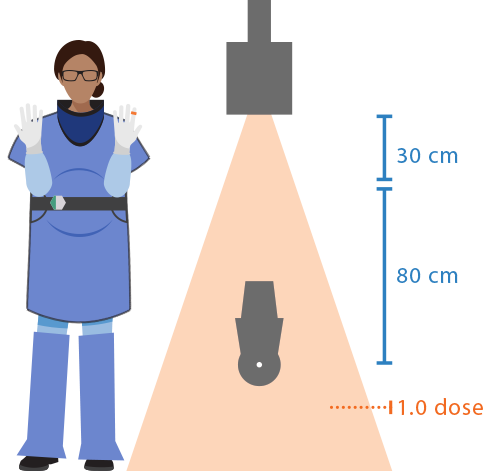
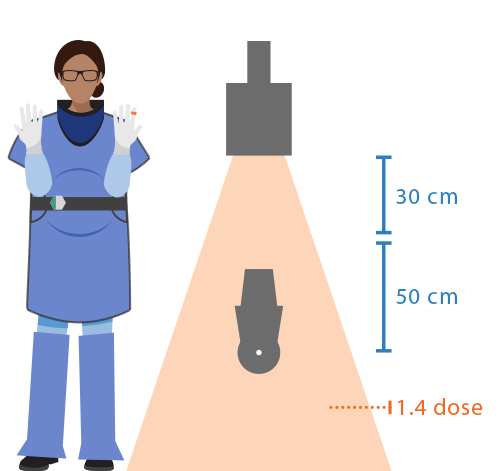
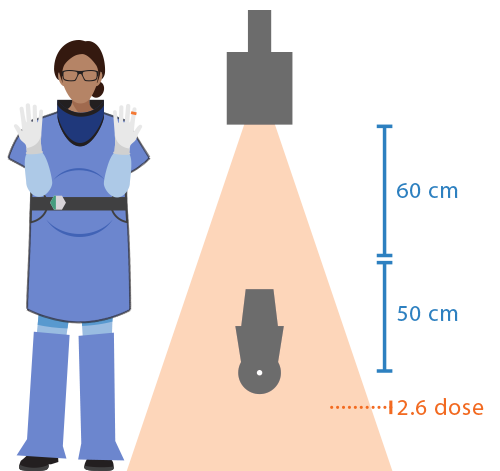
INCREASE THE DISTANCE FROM X-RAY SOURCE
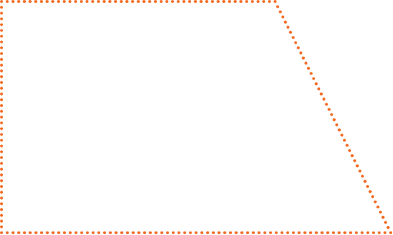
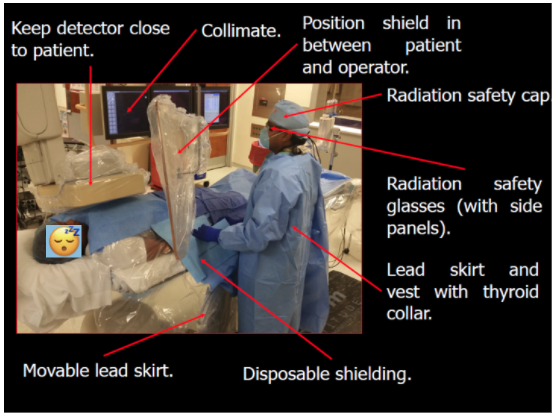
BLOCK SCATTERED RADIATION FROM THE PATIENT
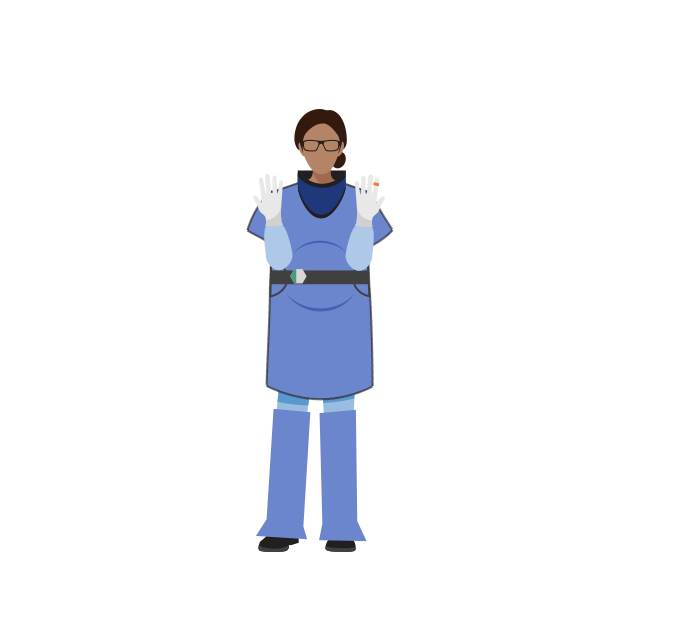
INTERVENTIONAL OUTFIT WITH ACCESSORIES
TABLE SET-UP
IMAGE ACQUISITION
BADGE MONITORING
Hirshfeld et al. 2018 ACC/HRS/NASCI/SCAI/SCCT Expert Consensus Document on Optimal Use of Ionizing Radiation in CV Imaging. J Am Coll Cardiol. 2018 Jun 19;71(24):2811-2828.
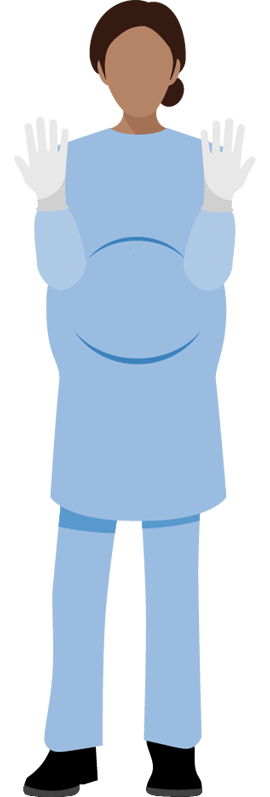
Leaded glasses
Shoulder Pads
Leaded apron
Radiation badge
Lead thyroid collar
Ring Dosimeter
Leg shields
Cathet Cardiovasc Diagn 1992;25(3):186-94.
Heart 2003;89(10):1123-4.
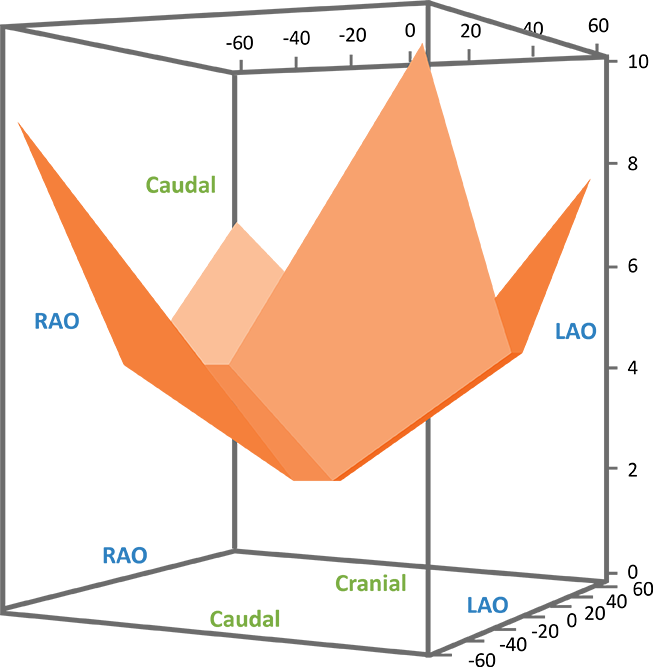
Drag to move the patient to view the radiation exposure results.



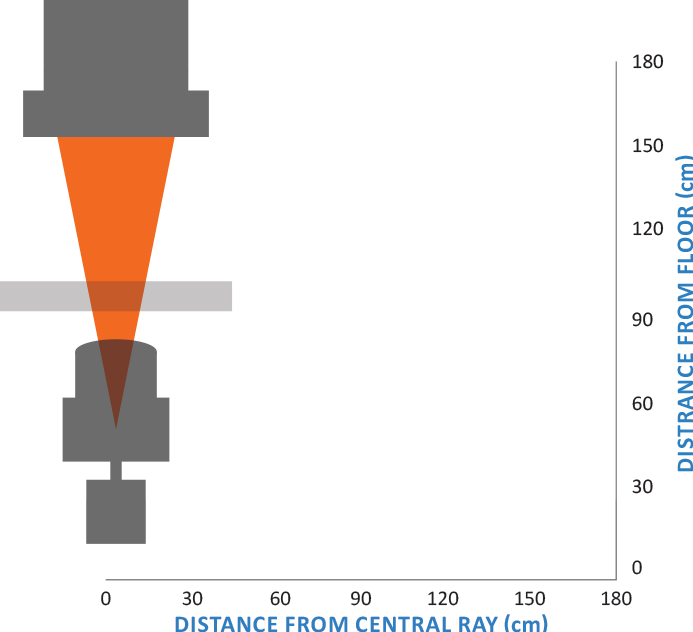
Slide courtesy of Dr. Patricia Best
Br J Radiol 1996;69:860-4.
Slide courtesy of Dr. Patricia Best